ICIJ’s mission is to reveal injustice and hold the powerful to account. Do you know of someone exploiting the coronavirus crisis, or have another story to share? We’d like to hear it. (Ici en Francais, aquí en Español)
It was easy to laugh off the United States President Donald Trump’s musings that disinfectants and sunlight might cure COVID-19.
But the comments, at an April 23 briefing, prompted state health authorities across the United States, as well as the manufacturers of bleach and Lysol, to warn the public not to ingest cleaning products, which are full of toxic chemicals that can kill. For good reason, as it turns out: poison control centers in New York, California and Maryland reported a surge in calls after the comments. Two men in Georgia reportedly drank disinfectants in an attempt to stave off the coronavirus.
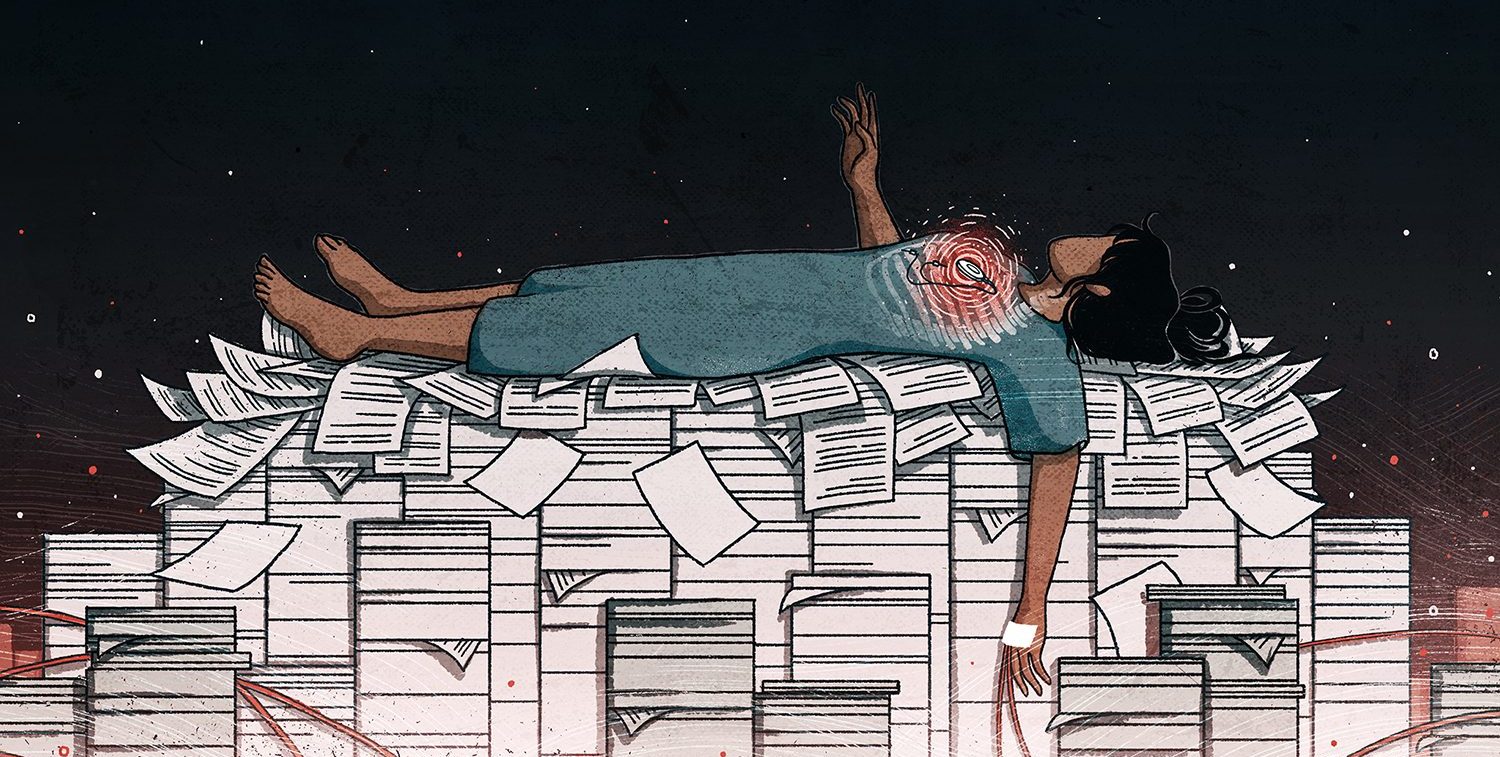
The incident was just one example of a broader and more dangerous phenomenon: the spread of unproven and sometimes dangerous treatments and tests for COVID-19.
The would-be coronavirus cures have varied from outlandish to promising but untested. For some of these products, rather than issuing alarms to protect public health, regulators and manufacturers have stood by or even encouraged their use. As a result, unproven treatments have been disseminated widely despite the absence of scientific data backing their safety and effectiveness.
“We’re in the Wild West in terms of the public susceptibility to unsafe, unproven drugs or tests that they hear about in the media or from political leaders,” said Lawrence Gostin, a professor of public health law at Georgetown University.
Gostin, who served on the World Health Organization’s expert advisory committee on the Pandemic Influenza Preparedness Framework, said that emergencies like COVID-19 can justify speeding up the approval process for new treatments.
As of May 1, the virus has claimed more than 230,000 lives worldwide, and more than 3 million cases have been detected. Doctors are desperate to aid patients with severe symptoms and there is no proven cure. An effective treatment would also help rescue battered economies, giving hope to a resumption of a more normal life.
The U.S. Food and Drug Administration has announced an accelerated approval program to hasten promising coronavirus treatments to market, shortly after suspending all routine inspections of drug and device manufacturing facilities.
One of the drugs reportedly fast-tracked for approval as a COVID-19 treatment by the FDA is remdesivir, which showed promising results in a recent clinical trial.
There’s zero justification for putting a drug or product on the market without reasonably rigorous testing – Lawrence Gostin
But, Gostin stressed, the pandemic does not eliminate the need for safety and efficacy reviews.
“There’s zero justification for putting a drug or product on the market without reasonably rigorous testing,” he said. “Full stop.”
In 2018, the International Consortium of Investigative Journalists’ Implant Files investigation found that broken or flawed medical devices were allowed on the market with little or no human testing, with devastating consequences. Regulators repeatedly bowed to pressure from device manufacturers to speed approvals and lower safety standards.
The coronavirus is different, of course: the pressure is coming from all sides. An effective medicine could save millions of lives. Yet the risks of moving too fast, with too little science, are the same as what ICIJ charted: treatments that could do more harm than the disease.
Here are some of the treatments and tests touted in recent months as effective without proof.
Avigan
The flu drug Avigan, produced by the Japanese company Fujifilm, has been embraced by several governments despite limited evidence that it works to treat COVID-19. The drug’s side effects may include increased risk of birth defects if it is taken by pregnant women.
Prime Minister Abe of Japan has been one of Avigan’s leading proponents. His administration has called for the drug, which has only conditional approval in Japan for serious infectious diseases such as Ebola, to be approved as a coronavirus treatment and for millions of doses to be stockpiled.
Abe is a personal friend of Fujifilm’s chairman Shigetaka Furumori.
Abe has lobbied heavily for the drug’s international use, including offering it for free to up to 20 countries through a grant to the United Nations.
China and Indonesia have been two of Avigan’s biggest users. A senior Chinese health official endorsed the drug in March as “very safe and clearly effective” after a trial on 200 patients, and Indonesia has imported millions of doses to treat its citizens.
At the same time, South Korea resisted its use, saying the evidence reviewed by its experts was unpersuasive.
“Avigan has not only not shown efficacy during test studies but also there is no data on clinical trials conducted on patients,” Oh Myoung-don, a South Korean infectious disease expert, told Yonhap news agency on April 4, weeks after China’s endorsement. “The drug has also shown serious side effects, such as fetal deaths in animal studies.”
Abe has reportedly lobbied Trump personally to promote Avigan in the U.S. The White House then pressed the FDA to approve emergency use of the drug as an experimental Covid-19 treatment, reported Politico on March 31.
On April 7, the FDA granted approval to three hospitals in Massachusetts to launch the first US clinical trials of Avigan.
Hydroxychloroquine and chloroquine
President Trump and several Fox News personalities promoted the anti-malaria drugs hydroxychloroquine and chloroquine as COVID-19 treatments for weeks, encouraging patients to try them out.
“I think it could be something really incredible,” Trump said on March 19.
Several weeks later, the hype fizzled. A trial conducted by U.S. government researchers among patients at the Veterans Administration found that subjects treated with hydroxychloroquine experienced no benefits and higher death rates than patients who received standard treatment. The drug’s side effects included an increased risk of potentially lethal heart failure.
A few days later, the FDA issued a safety communication warning against the use of both anti-malaria drugs for COVID-19.
In the interim, the drugs were widely disseminated not only in the U.S. but internationally – posing risks that have so far have not been investigated or quantified.
By the evening of March 19, when Trump first used his White House telecast to pitch hydroxychloroquine and chloroquine, first-time prescriptions of the drugs flooded pharmacies at 46 times the average weekday rate, a New York Times analysis found. On March 29, the FDA issued an emergency use authorization for both drugs, and millions of doses were donated by their manufacturers to the U.S Strategic National Stockpile for Covid-19 treatment.
In at least two cases, doctors or public officials have sought to use the drugs among highly vulnerable populations.
At a nursing home in Texas, the medical director gave hydroxychloroquine to elderly Covid-19 patients in what he called an “observational study.”
And in the slums of Mumbai, India, city officials developed a plan to administer the drug to thousands in a mass test to determine its effectiveness as a preventive medication. The plan has now been temporarily put on hold.
The anti-malaria drugs were also used widely by physicians and hospitals, in some cases even before President Trump’s recommendation. By late March, the demand for the drugs was so intense that patients with lupus and arthritis, for which they are FDA-approved treatments, were often unable to obtain them at pharmacies, placing them at risk of withdrawal symptoms and flare-ups that could result in hospitalization.
Antibody tests
A key tool for reopening economies is antibody testing – blood tests that assess whether individuals have had COVID-19 and are immune to future infections.
Under pressure to speed the U.S. recovery, the FDA approved about 90 companies, mostly from China, to sell antibody tests without government vetting. The result has been a flood of flawed products that have placed the public in danger due to high rates of inaccuracy, the New York Times reported on April 19.
Among the approved products were tests used in Laredo, Texas, which the local health department found to have only 20 percent reliability. The manufacturer had claimed the tests were 93 to 97 percent accurate.
In New York City, the epicenter of the U.S. epidemic, the health department sent out a letter to health providers on April 22 warning them against relying on any existing antibody tests to determine patients’ COVID-19 immunity.
“They may produce false negative or false positive results, the consequences of which include providing patients incorrect guidance on preventive interventions like physical distancing or protective equipment,” wrote Deputy Commissioner Dr. Demetre C. Daskalakis.
The smoke cure
While some political leaders have embraced unproven drugs or testing products, others have denied the crisis altogether.
Brazil’s Jair Bolsonaro has dismissed the coronavirus as “a little cold” and fired his health minister for promoting social distancing. Nicaragua’s Daniel Ortega has refused to shut down businesses or public events, and his government held a mass rally in April dubbed “Love in the Time of COVID-19.”
In Turkmenistan, the eccentric despot Gurbanguly Berdimuhamedov has charted another course entirely. He ordered his government to fumigate the country with smoke from burning a traditional herb called harmala, which he said would destroy the viruses.His ministers praised the move, noting that Berdimuhamedov had written about the herb in his book Medicinal Plants of Turkmenistan.