For the past decade, European lawmakers have been at the center of a lobbying storm.
Bold plans to overhaul safety regulations for the millions of medical implants embedded in patients each year — including artificial hips, breast implants, stents, defibrillators, and pacemakers — have been wrecked by an army of lobbyists. Not once, but twice.
A year-long investigation by the International Consortium of Investigative Journalists and 58 partner news organizations in 36 countries, known as the Implant Files, has discovered how top European Union politicians and officials were won over by misleading claims from implant industry lobby groups.
These claims played a pivotal role in shaping the course of EU policy and killing off any prospect of a fundamental strengthening of medical device regulation, first in the European Commission and later in the European Parliament.
Public health campaigners say Europe is in urgent need of tougher rules. Even though millions of Europeans’ lives have been lengthened or improved by medical devices, the EU has borne the brunt of many of the world’s worst implant scandals, unnecessarily leaving many patients scarred, in agony or even dead. Leading surgeons, regulators, lawyers and campaigners have said Europe’s approach to evaluating and approving new implants means that its citizens are treated “like guinea pigs.”
The Implant Files is a year-long investigation coordinated and reported on by ICIJ, involving more than 250 journalists from 36 countries, into the behaviors of the medical device industry around the world. It traces rapid advances in device technology and reveals safety regulations have struggled to keep up. Meanwhile, investor pressure on companies to grow profits has sometimes clashed with the best interests of patients.
Investor attention is often trained on the time it takes regulators to approve new products. Larry Biegelsen, at Wells Fargo, is among many Wall Street analysts to have identified a quickening pace of approvals in the United States in the last three years. In a research note published in June, he said this had led to more patients being treated, to rising sales and profits and ultimately to stock prices that have outperformed the rest of the market. “We’re calling [it] a virtuous cycle of innovation,” Biegelsen said.
To get new products onto the market even quicker, however, many medical device firms travel first to Europe, which has some of the lightest regulations in the developed world. Lobbyists celebrate the EU approach as “a new international paradigm”. The industry’s largest trade association in the region, MedTech Europe, said EU rules had influenced safety regimes in Canada, Japan and Australia. More recently, industry lobbyists in the U.S. have pressed regulators to adopt ideas from Europe.
The patients became the test subjects for these companies and that’s why I feel like a guinea pig. – Jurgen Thoma
Some other countries have done more than borrow regulatory ideas from Europe. The authorities in Saudi Arabia, India, the Philippines, Singapore, Israel and much of Latin America wave through devices, or subject them to less scrutiny, if they have already been certified as safe in Europe.
Jürgen’s hip
Although the global implant industry is dominated by U.S. manufacturers, and America is by far the largest sales market, many firms choose Europe to try out their new — and sometimes dangerous — products.
This is done long before these novel devices have been tested to the satisfaction of the U.S. Food and Drug Administration. Manufacturers are drawn by Europe’s less exacting regulations that allow new devices to be quickly approved as safe for use.
In 2005, Jürgen Thoma was a 48-year-old technical manager at a large winery close to Freiburg, in the south of Germany, when he became one of millions of European citizens to receive an implant made by an American firm but not yet cleared as safe by the U.S. FDA. His right hip was replaced with an all-metal joint manufactured by Zimmer Holdings (now Zimmer Biomet) of Warsaw, Indiana.
Under European regulation, the hip was certified as safe for use in 2003 without Zimmer having to provide clinical evidence of safety. Instead, the U.S. firm was able to argue its new hip design was sufficiently similar to others already on the market.
Before long, Thoma said, the new hip was causing him pain. Metal debris was wearing off of the hip and worming its way into the surrounding tissue and bone. In 2009, he underwent surgery to have the hip replaced. Surgeons found a festering infection in the bone which had turn grey and caused softening. Thoma said it looked “like a porous sponge, like Swiss cheese – that’s how the bone is eaten up.”
He believed Europe’s safety rules had let him down, and began a court case against Zimmer. Thoma told ICIJ media partners: “The patients became the test subjects for these companies, and that’s why I feel like a guinea pig… I am an engineer. I often put components into machines, but they have to last.”

Last month, a judge in Germany ruled in his favor, saying the Zimmer hip “should not have been put on the market.” After an eight-year legal fight, he won just €25,000 in damages (equivalent to $28,600) for injuries suffered, impaired health and the ordeal of corrective surgery – a big payout by European standards. Zimmer denies Thoma’s artificial hip was defective and last week filed an appeal.
Suspect injuries, malfunctions and deaths
Thoma is lucky compared to some. Many patients with similar stories spend large sums on court cases that fail, thanks to personal injury liability laws in Europe that are more industry-friendly than those in the U.S.
Like Zimmer’s metal hip, many more products were developed by U.S. manufacturers before receiving their first safety approval in Europe. They include PleuraSeal, a lung sealant that leaked; RoboDoc, a robotic surgical device that caused tendon rupture and nerve damage; and Brio, a deep brain stimulation implant to treat Parkinson’s disease, which had to be removed from some patients after body fluids seeped into the device and it stopped working.
In addition European patients were the first to try Nanostim, a breakthrough pacemaker, able to function without leads, some of which developed battery problems; and Trilucent, a breast implant filled with soybean oil, some of which went rancid, prompting regulators to recommend that thousands of women undergo surgery to have them removed.
Each of these devices was eventually recalled, put on hold or discontinued.
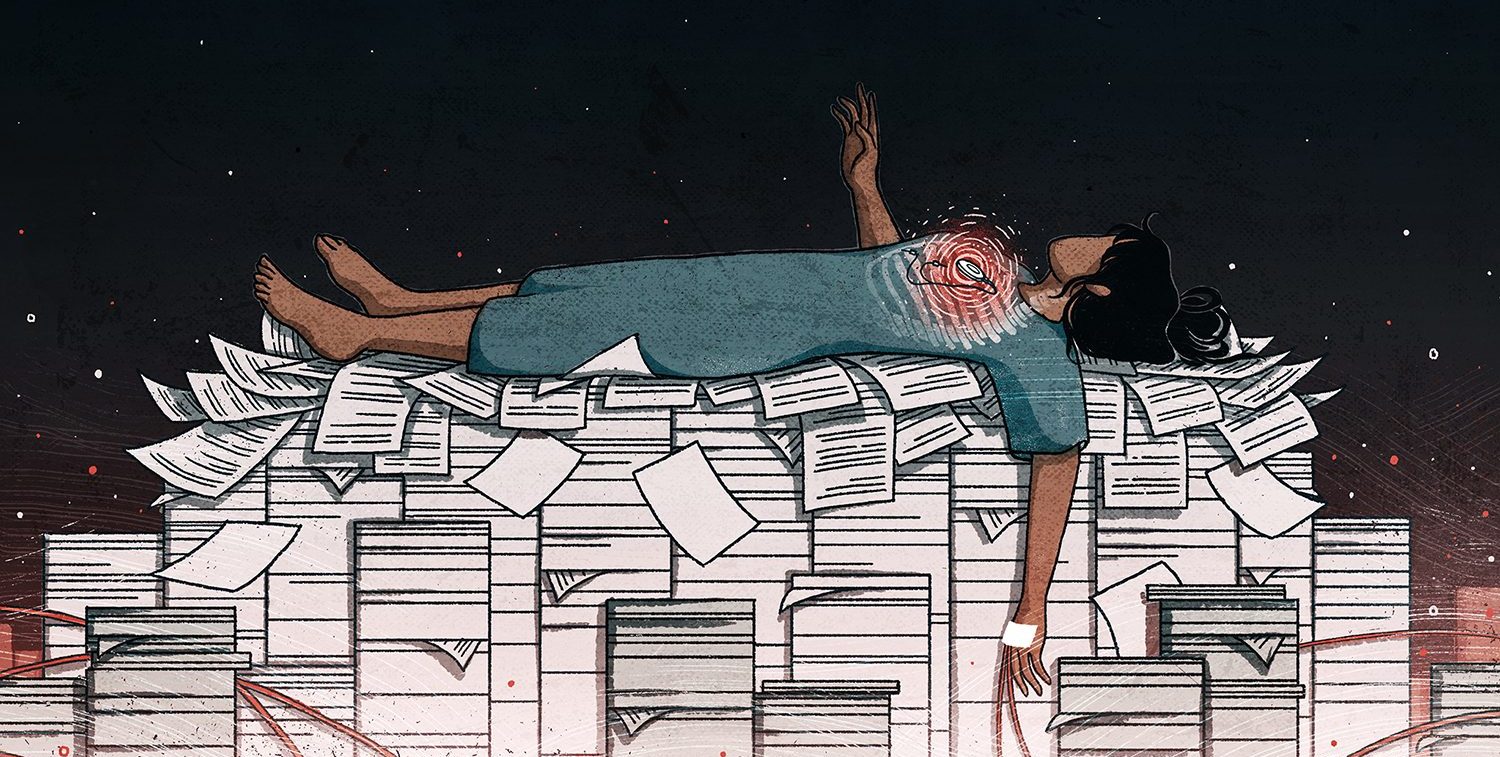
Despite the exposure of European patients to dangerous devices, official regulatory statistics often fail to capture their stories. Not all manufacturers learn of injuries associated with their products. When they do, companies are required to file an “incident report,” indicating that a device may have caused serious harm or put a patient in danger. However, circumstances often allow manufacturers latitude to exercise judgment over whether or not to file a report.
Despite their limitations, incident reports offer the best-available view of potentially dangerous medical products in use in Europe. Yet national health authorities refuse to make them public.
ICIJ reporting partners in 16 European countries have spent months seeking access to detailed injury and malfunction data held by national regulators. But in each case, freedom of information requests were denied or led to incomplete responses, full of redactions.
In Belgium, regulators said it would take one person 5,489 days to black out patient data or commercially sensitive information before requested documents could be released. In the UK, reporters tried asking only for those injury reports relating to Essure, a sterilisation implant known to have harmed many women, but were told this would violate the manufacturer’s commercial secrecy.
Regulators in 19 countries – responsible for the safety of more than 85 percent of EU citizens – did respond, however, to an ICIJ request for the raw numbers of reported malfunctions, injuries and deaths. The data they provided shows a steep rise in incident reports over recent years.
In Germany, confidential reports have almost tripled in the last nine years. The 72 officials who oversee the country’s device regulation last year received 14,034 suspected device-associated injury and malfunction reports – equivalent to 54 reports every working day – including 224 reports of death.
In France and the UK, incident reports have more than doubled in nine years, reaching 18,208 and 19,559 respectively. In Spain, they have quadrupled in seven years, while in Italy reports quadrupled in just four years.
Without more detailed data – such as the number of different devices on the market and how frequently they are used – it is impossible to know whether the rising number of injury and malfunction reports means products are getting more dangerous.
However, several countries – including the UK, Italy and the Netherlands – said sharp increases in part reflected improved reporting practices. In the recent past, they explained, manufacturers had been under-reporting incidents involving their products.
Dr. Christian Gluud, head of the Copenhagen Trial Unit in Denmark, said keeping incident reports confidential was effectively an “expropriation” of information belonging to patients, which should be shared openly in the interests of public health.
“To me, this looks totally medieval,” he said. “It should be urgently changed. We need much more transparency. Only if patients and doctors have full access to all the benefit and harm data can they make informed decisions on whether to use a particular medical device.”
Although the EU is currently reviewing how much information should be shared with the public on a newly expanded computer system called Eudamed, the European Commission told ICIJ that injury and malfunction reports were likely to remain confidential as they were commercially sensitive for manufacturers.
Ronald Boumans, a technical adviser helping the Commission develop Eudamed, said he found this “personally disappointing” but explained that the authorities feared manufacturers would be less willing to share reports about accidents potentially caused by their devices if that information were made public. “This is the fine balance between getting everybody to report and giving the public access to data,” Boumans said.
Until Eudamed is fully upgraded, no single authority even keeps a register showing the number of medical devices certified as safe for use in Europe. Regulators in some countries told ICIJ they believe there are about 500,000 devices on the EU market.
But according to evidence given to the U.S. Institute of Medicine for its 2010 report on medical device regulation, the EU figure at that time was more likely 750,000, which compared with less than 10,000 active pharmaceuticals. Meanwhile, devices are also updated regularly, with many products being superseded by updated models or new devices within two years, making regulation a daunting task.
Light-touch Europe
For nine years, lobbyists pressured politicians as they wrote and rewrote plans to reform Europe’s safety rules, before legislation – known as the Regulation on Medical Devices – was finally signed into law last year, ready to come into effect from 2020.
The process spanned the tenure of two commission presidents, three parliaments and 11 changes to the presidency of the EU Council, the body which together with the parliament passes laws. Meanwhile the medical devices brief passed down through four successive health commissioners before ending up with the EU’s commissioner for industry.
Throughout, lobbyists fought to keep as much as possible from the EU’s existing, light-touch safety regime. For more than two decades, it had allowed private, for-profit certification firms, known as “notified bodies,” to approve high-risk products, including pacemakers, stents, breast implants and artificial joints, as safe — often without any supporting evidence from trials in humans.
The battle over how medical devices should be regulated offers a window in to how well-connected lobbyists can overwhelm a process designed to protect the public. Lobbyists won over European politicians and bureaucrats with an array of tactics, including not only unsubstantiated claims about safety but also and dark warnings of lost jobs, increased taxes and fewer healthcare choices.
At the moment, the only assurance of safety given to doctors and patients before an implant is inserted is the small “CE” logo on the packaging or instructions, which the patient may never see. It is the same “Conformité Européenne” mark, certifying that “essential requirements” on safety and environmental protections have been met, that appears on many consumer goods sold in Europe, including toasters, fireworks, and children’s toys.
A disliked proposal
In 2008, European Commission officials had become aware that notified bodies, vying with one another for business, were routinely awarding CE certificates for new, high-risk implants without being shown supporting evidence. Patient safety was at risk, the Commission said, and the EU needed “fundamental” changes that would “recast the entire medical device framework”.
As a solution, the Commission produced a range of options, including transferring responsibility for assessing high-risk devices, including implants, to a new department within the European Medicines Agency “on an equal footing” with the EMA’s work regulating drugs.
In both Europe and the U.S., all new drugs must undergo carefully designed trials in human test subjects indicating an acceptable level of safety and effectiveness. Rigorous tests are also required for very innovative new devices in the U.S., but requirements for such products in Europe are less demanding.
Commission proposals for rigorous testing overseen by the EMA brought a barrage of 200 responses, including 117 submissions from manufacturers, industry trade associations, notified bodies, consultants and experts, 27 from government regulators and just 33 from healthcare workers and academics. The vast majority of respondents were against involving the EMA, but there was a clear split between industry and the notified bodies, which firmly rejected the idea, and doctors, academics, patients and consumers, who were largely in favor.
The Irish Medical Devices Association, a trade association whose members include global corporations such as Medtronic, Allergan and Abbott Laboratories, said it did not agree with the commission’s analysis of weaknesses in current regulation. “The device industry … sees no evidence of either the alleged problems or the reasons why [the EMA] would present the appropriate solution if those problems did indeed exist.”
If the commission’s proposals were taken forward, warned MedTech Europe, “patient care and access to new medical technology is, in our view, likely to suffer.” Options under consideration, the lobby group added, were “alarming”, “objectionable” or “completely unacceptable”.
Ranier Technology, of Cambridge, England, a maker of artificial spinal discs, sent the commission its thoughts in a single sentence. The proposals were, it said, “trying to fix a problem that doesn’t exist.”
Scandals and loopholes
This emphatic response might have been the end of the matter. Then two high-profile scandals surfaced, beginning in 2010.
French regulators discovered that tens of thousands of women had received breast implants that were susceptible to rupture. The implants had been illegally filled with industrial grade silicone as a cost-saving measure by French manufacturer Poly Implant Prothèse (PIP), triggering a huge public uproar. In France alone, more than 18,600 women had PIP implants surgically removed in the wake of the scandal.
Meanwhile, several makers of all-metal hips stopped production, acknowledging that these implants – popular with younger patients – were in fact failing at alarming rates.
In the midst of the scandal, investigative journalists at the medical journal BMJ and The Telegraph in the U.K. went undercover, posing as representatives of a rival hip manufacturer and asking Slovakian notified body EVPU to provide a CE mark, certifying their new all-metal hip as safe.
EVPU were secretly filmed explaining that its “price is good” and that its certification work was “very fast”. Later, the Slovakian firm provisionally approved the journalists’ hip design, which had been deliberately drafted to mirror that of a dangerous hip product that had been subject to a safety recall.
Around the same time, other notified bodies were helping manufacturers by stretching the rules in different ways. In 2012, Maikel Hendriks, a Dutch engineer and specialist in regulation, became the first person to have a cranberry-based pill, purporting to treat women with urinary tract infections and cystitis, classed as a medical device.
Rival companies, including Ocean Spray, the Massachusetts-based fruit grower, had been banned from claiming that their cranberry products were similarly effective after a series of decisions by the European Food Safety Agency. But Hendriks was free to make otherwise prohibited treatment claims because his new pill, called i-Say, was not regulated as a food supplement.
Instead, ECM, a notified body in Aachen, Germany, provided Hendriks with a CE certification, which was all he needed to make medical claims for his cranberry capsules.
Several competitors soon brought out similar cranberry “medical devices,” approved by notified bodies in France and the U.K., much to the frustration of urologists.
This loophole continued until last year, when the commission ruled that the active ingredient in cranberry pills could not be a device, because – regardless whether or not they were an effective treatment for cystitis – it behaved more like a drug than a device. Hendricks claims the ruling does not apply to his i-Say products, but many pharmacy chains are now reluctant stock it.
Other tablets have also been classified as medical devices including slimming pills XLS-Medical Fat Binder, Hunger Buddy and Fat Blaster. Again, the EFSA has made critical comments about the effectiveness of ingredients in some of these tablets, but these opinions can effectively be ignored so long as the products are classed as medical devices.
Hendriks thinks there are further opportunities to reclassify many commonly used pills as devices. “I’m willing to make a bold statement,” he told ICIJ. “I think 5 percent of drug-registered products should not be registered as drugs, but should be medical devices.”
Changing course
Spurred by public outrage, in 2012 the European Parliament, which would have to approve any changes in medical device rules, called on the commission to renew efforts to overhaul safety regulations.
But when new proposals finally emerged from the commission in 2012, they looked very different from what the same organization had proposed in 2008.
According to an official “impact assessment,” deeper research had led the commission to conclude any weaknesses in the system “do not suggest that [the regulation of medical devices] is fundamentally unsound.” There was no need to stop notified bodies from approving the safety of implants and other high-risk devices, or to transfer that task to the EMA.
The commission explained that it had held “targeted meetings at [a] senior level with representatives from industry associations and with Notified Bodies.” Several fact-finding events had taken place, but records show they were dominated by industry lobby groups, with few independent medical specialists present and even fewer patient groups. Meanwhile, countries where lots of jobs depended on medical device firms, including Germany, the U.K. and Ireland, began to line up in support of industry.
The commission’s official 80-page impact assessment explained how a new, centralized regulator was now deemed “inappropriate.” It would have enormous impact on the EU budget, on manufacturers and on innovation, officials wrote.
Parroting the lobbyists, they explained how current regulations allowed device makers to get cutting-edge new technologies into European hospitals for a cost of less than 10 million euros. The cost for heavily regulated pharmaceutical firms to develop a new drug was about 1 billion euros.
The case for rejecting tougher safety regulations was overwhelming, the commission document concluded. Most importantly, it said, such a move would bring with it no safety benefits for European citizens. “U.S. studies… point to the faster pre-market assessment in Europe compared to FDA clearance of medical devices, whilst safety levels were considered equal,” the impact assessment explained.
As the footnotes made clear, these were studies by Boston Consulting Group.
The consultancy firm’s work was not quoted, but it had been accurately summarized. One Boston Consulting report, which compared the number of products recalled because of serious risk to patients, had indeed concluded: “[T]he number of recalls in Europe is identical to that in the United States.”
Another, jointly written by Boston Consulting and the industry-funded California Healthcare Institute, said: “For complex medical devices … the EU system has consistently offered a faster route to market.” Again, it added: the “average rate of recall in Europe … is almost identical to the rate of equivalent recalls in the U.S.”
‘Inappropriate’ evidence for policy making
What the commission document did not mention, however, was that Boston Consulting’s work had been paid for by industry lobby groups, and that its findings had been used once before to influence policymakers. Not in Europe, but thousands of miles across the Atlantic in Washington, D.C. – where they had attracted sharp criticism.
In 2011 David Nexon, senior executive vice president of AdvaMed, the U.S. device industry trade association, appeared before a U.S. Senate committee reviewing the performance of the FDA. He complained that high-risk medical devices took three years longer to be approved for use in the U.S. than in Europe.
This “disturbing pattern of delay and inefficiencies” was depriving patients of ready access to treatments and cures without improving safety, Nexon argued. He, too, cited the Boston Consulting reports.
But the reports drew a sharp rebuttal from House Democrats, who published a memo raising what they called “significant questions about their methodologies and their appropriateness for serving as the basis of new policies governing the medical device approval process.”
To back up their point, the Democrats included the views of the editors of several leading medical journals, all of whom were critical of Boston Consulting’s work.
Dr. Rita Redberg, a cardiologist and the editor of the journal JAMA Internal Medicine, wrote that it had assumed “the faster the FDA approves a device, the better. That may be true from the perspective of a medical device company but it is not true from the perspective of patients.”
Earlier, Dr. Jeffrey Shuren, the FDA’s head of medical device regulation, had hit out at separate claims that European regulation was superior. “We don’t use our people as guinea pigs in the U.S.,” he said.
In May 2012, the FDA published what amounted to another rebuttal: a document called “Unsafe and Ineffective Devices Approved in the EU that were Not Approved in the US.” Listing a dozen examples, the FDA said: “Most of these devices were ultimately withdrawn from the EU market, but only after thousands of patients were harmed.”
In Europe, however, many politicians were more willing to accept Boston Consulting’s findings, a summary of which became a mantra for many. A briefing note prepared by commission officials, for instance, counseled then-EU Commissioner for Consumer Protection Neven Mimica how to respond when asked why the EU had dropped proposals for the European Medicines Agency to step in and regulate implants. The note recommended this language: “It would be detrimental to innovation and competitiveness without any demonstrated added value for patient safety.”

An emotional appeal
By 2013, implant lobbyists still faced considerable challenge among members of the European Parliament.
An experienced parliamentarian in Germany’s Social Democrat party, Dagmar Roth-Behrendt had long been interested in medical issues and says she always saw device regulation as the “missing cornerstone” in European health law.
“When I saw the proposal from the commission I knew that it would not solve half of the problems we have Europe-wide,” she told ICIJ partners. “So, I tried to start, more or less from scratch, to write the legislation new again.”
Knowing it would be a challenge to win a majority in parliament, calculated compromises were made as she wrote out hundreds of amendments to the commission’s plan. “I tried to go as far as I could [while] still watching myself in the mirror each morning.”
In the end, her alternative proposal once again sought to bring forward the idea of a central EU agency to evaluate high-risk implants. She also wanted to require manufacturers to demonstrate that devices were not just safe but actually delivered a benefit to patients.
In advance of a crucial 2013 vote on the Roth-Behrendt plan, MedTech Europe launched an online lobbying campaign, once again relying heavily on Boston Consulting’s claim that the latest cutting-edge implants were approved three years faster in Europe without additional risk to patients. The campaign’s catchphrase was: “Don’t lose the 3.”
The website said: “Certain voices in Brussels are calling for radical changes to the system that would dramatically slow it down and unnecessarily delay life-saving medical devices reaching patients.”
On the homepage was a video featuring an actor playing “Florence,” a patient with dangerously high blood pressure for whom drugs were not helping.
“Having medical devices regulated by one central agency will cause unnecessary three-year delays,” the narrator intoned, emphasizing the word “will,” as the actor shuffled down a hospital corridor in a robe. “Florence doesn’t have three years.”
Existing EU rules meant Florence’s treatment – delivered using a novel catheter-based device that removes overactive nerves deep in the kidney – had been available in Europe since 2010, according to the campaign website, which has since been taken down. On the site, MedTech Europe said seven million U.S. patients in a similar condition were still waiting for the FDA to approve the treatment that they, and Florence, needed.
The lobbyists claimed Roth-Behrendt’s reforms would cost industry 17.5 billion euros ($20 billion) and would make European citizens no safer than they were before.
Although the Parliament had been divided shortly before the October 2013 vote, Roth-Behrendt’s push for fundamental reforms was ultimately defeated.
“I saw a huge amount of lobbying in the 25 years I was in the European Parliament,” Roth-Behrendt told ICIJ partners. “But the way this was done was the blackest I’ve ever seen. And I wonder that people can get along with their conscience.”
Just three months later, in the U.S., the first thorough clinical trial of the device MedTech Europe said could save Florence’s life was completed.
The study involved 535 patients in 87 U.S. medical centers, two-thirds of whom were treated with a Medtronic device called Symplicity while the remaining third were given a sham treatment. The trial was carried out because the FDA would not approve the denervation device for use in U.S. hospitals without scientific evidence it was effective.
The result suggested the cutting-edge technology – estimated to cost nearly $4,000 per patient and supposed to revolutionize high blood pressure treatment – was useless.
“This blinded trial did not show a significant reduction of … blood pressure in patients with resistant hypertension six months after renal-artery denervation as compared with a sham control,” the lead investigators explained.
Further patient enrollment in trials in the U.S., Japan and India was suspended by Medtronic, which was forced to reduce the value of the technology in its financial statements by $236 million. Rival manufacturers responded by winding down their efforts to develop competitor devices, though since then some firms — including Medtronic — have attempted to improve the technology and believe it eventually will be of value to some patients. Medtronic told ICIJ it now believes 2014 poor trial results were the result of flaws in the design of the trial, not in the effectiveness of the device.
Asked if, with the benefit of hindsight, it had overstated the benefits of the denervation device used to treat Florence, MedTech Europe declined to answer. “We provide input to policymakers to support their understanding of our industry,” it said in a statement to ICIJ: “[We] hope that this information will help them shape a sustainable and appropriate regulatory environment that better serves patients.”
Roth-Behrendt told ICIJ media partners: “It makes me very frustrated when I see that a device used in that smear movie … is now not even effective.” She added: “I was not sure if I should cry or laugh … It was so disgusting, way below the belt. But this is how the lobbying worked and many MEPs [members of the European Parliament] fell for it.”
A victory for lobbyists
While the EU’s new safety regulations were not signed into law for another four years, any hope for fundamental reform died with Roth-Behrendt’s failed efforts in the parliament.
When the text was finally agreed upon last year, Commissioner Elżbieta Bieńkowska, whose internal market department holds responsibility for implant regulation, claimed it was a victory for patient safety. “I am extremely happy that our push for stricter controls of medical devices … will now become a reality.” Dr. Vytenis Andriukaitis, the EU commissioner for health and a retired cardiac surgeon, said he “happily welcomes the final compromise, which contains a series of crucial improvements to the current system.”
Glenis Willmott, who succeeded Roth-Behrendt as the European Parliament’s point person for tracking and reporting on medical devices law, blames the failure to secure more fundamental reforms on her centrist and right-wing peers. Roth-Behrendt agrees.
“I would have liked to have seen an end to the direct financial relationship between medical device manufacturers and the notified bodies which assess them, but this was also not politically achievable,” Willmott reflected, noting that other opportunities were also missed.
Willmott, now retired from politics, said the legislation ultimately represented a compromise, including some valuable measures. Like Commissioner Andriukaitis, she pointed to the new powers to appoint a panel of experts that will, in some instances, double check the work of notified bodies and to a new requirement for all implants to be given an identification number to help keep track of them. These measures were “a big step forward,” she said.
Europe’s rules are all about helping companies to sell more implants — they are nothing to do with public safety. – Alain Braillon
Not everyone agrees. Carl Heneghan, professor of evidence-based medicine at Oxford University in the U.K., said: “The new device regulations give the impression of creating safer devices, but more regulation does not necessarily mean better regulation.” He said they amounted to “a hundred pages of smoke screen.”
Dr. Alain Braillon, a senior consultant at Amiens University Hospital and health products expert, said: “Europe’s rules are all about helping companies to sell more implants — they are nothing to do with public safety. The European Union is a political union firstly aimed to ensure the free movement of goods, services and capital.”
Kurt Racké, a leading member of the German association of medical research ethics committees, said: “In my opinion the new [legislation] fails to make the medical device approval process safer. The requirements have not been changed tremendously in comparison to the old legislation.”
Most angry of all was Roth-Behrendt. “Medical devices must be safe and reliable. That hasn’t been achieved in the past, and it won’t be in the future,” she said. “With medical device scandals happening, those lawmakers and decision makers who have prevented better regulation or watered it down should explain themselves. Why did they not [do more] for more patient safety?”
Industry trade bodies, meanwhile, declared victory.
At a conference in Berlin, Dario Pirovano, a senior figure at MedTech Europe who had worked as a consultant for the commission earlier in his career, gave a PowerPoint presentation that listed industry successes, including some big ones.
He noted that proposals for an EU public authority to assess safety, similar to the FDA, had been scrapped and a proposal to require testing for efficacy — as is required in the U.S. — had been rejected.
Other “major blockers to innovation” had been “deleted or balanced,” Pirovano said.
For the MedTech Europe industry group and for its members, he declared, EU’s new regime was a “positive result.”
In 2016, BMJ published an independent, peer-reviewed study examining the safety record of medical devices approved for use in both the U.S. and Europe. The study compared the safety profiles of 206 new devices approved in both America and the EU over a six year period. It found that those “approved first in the EU were… associated with a nearly threefold greater rate of safety alerts and recalls.”
ICIJ asked Boston Consulting if it accepted the findings of the BMJ study, and for a response to criticisms of the methodology used in its own work. The consultancy firm declined to comment.
ICIJ asked the EU commission about the different conclusions reached by Boston Consulting and the BMJ study. In a statement, it said: “A comparison between the US and new EU legislative framework would require a more detailed discussion. Different analyses come to different conclusions and generally recognize that each of the two systems has specific benefits.”
It added: “The Commission always acts in the European interest, not in the interest of any one group or stakeholder. In reforming the system of medical devices, commercial interests were never prioritized over patient health.”
‘Unnecessary worries’
Although Europe’s new safety rules have been passed into law and will come into effect beginning in 2020, some of the most controversial issues have been left hanging, to be resolved at a later date in “implementing acts.” One major remaining concern: how much should doctors and the public be told about devices? For many physicians, the benefits of knowing whether or not a new product has been through rigorous testing are obvious.
Alan Fraser, a cardiologist and professor at the University Hospital of Wales, in the UK, said: “We’re arguing that there should be specific requirements… to ensure that regulators give access to the evaluations [of medical devices] by notified bodies — just as you would get such information for new drugs.”
Similarly, many public health experts see a clear advantage in being able to analyze the tens of thousands of injury and malfunction reports that are submitted to regulators in European countries each year.
For many years, there have been question marks over the integrity of incident reports. During the PIP scandal, it emerged that some regulators had for years been concerned about French company’s “tendency to draw inappropriate conclusions” when filing reports on women who had had their implants removed. Incident reports from PIP regularly presumed implants that were cut open or torn must have been damaged by the surgeon carrying out the explant procedure.
Regulators in Italy told ICIJ partners that under-reporting was “known and widespread throughout Europe,” though they claimed to have taken steps to address the problem.
In the U.S., the FDA keeps a public register of such reports, available for doctors, patients and academics to search. Under new EU rules, however, regulators are expected to continue to hold similarly detailed information confidential.
While a formal decision had not yet been announced, the commission told ICIJ that publishing details of patient harm possibly caused by medical devices would scare the public. A spokesperson said there was a need “to avoid unjustified mistrust and concerns.”
A 2015 internal commission memo suggests there may be more to this policy decision than a desire to avoid unnecessary public worry. It reveals that EU officials met with MedTech Europe lobbyists who warned them that Europe could lose out on investment if its new regulations insisted on greater transparency.
The memo records the lobbyists asking EU officials for more detail on “the relationship to be established between transparency needs and protection of commercially sensitive information.” For MedTech Europe, the memo explained, “clarifying this adequately … is crucial to make sure that [Europe] remains fit for attracting innovation and research investments.”
Race to the bottom
In April 2017, after its victory in Europe, the device industry turned its attention to the world’s largest healthcare market, the U.S.
Here, regulation had begun to slowly adopt elements of Europe’s more hands-off system. The FDA has introduced rules to work more closely with private certification companies and give greater weight to safety standards developed by industry.
Last year, another official from trade group AdvaMed again appeared before a Senate committee to give his view on the agency’s performance.
“I’ve been encouraged by progress at FDA’s device center in recent years, but the innovation ecosystem that supports our industry remains stressed,” said Scott Whitaker, chief executive of AdvaMed. “The time horizon for getting a new innovation from the bench to the bedside remains too long.”
In response to industry arguments, Shuren, the FDA’s regulatory chief over devices, promised the agency would cut the time it takes to evaluate the safety of high-risk implants by one-quarter over five years.
And in a blog post, he and Dr. Bram Zuckerman, an agency colleague, said the FDA was ready to compete with Europe on approval times. “U.S. medical device companies have long been accustomed to going overseas… securing marketing authorization in other countries, and then returning to the U.S. for pivotal clinical trials before FDA approval,” the FDA officials he wrote.
“We’re trying to break that model.”
Contributors: Stéphane Horel, Jet Schouten, Petra Blum, Deborah Cohen, Kristof Clerix, Cecile S. Gallego, Andras Petho, Anuška Delić, Ola Westerberg, Joop Bouma, Colm Keena, Christian Baars, Frederik Obermaier, John Hansen, Minna Knus-Galan, Giulio Valesini, Nina Selbo Torset, Daniele Grasso, Marie Parvex, Cataldo Ciccolella, Elena Kuch and Arne Hell