Jeanne McArdle was 85 when her doctor said that she needed her heart valve replaced.
Not long before, her best option would have been open-heart surgery, to cut out her valve and sew in an artificial one. McArdle was happy to learn that doctors had recently come up with a new kind of fix: a minimally invasive procedure called transcatheter aortic valve replacement, or TAVR. Instead of surgery, a new valve could be inserted through a small incision and then into the heart on the end of a thin, flexible tube called a catheter. The procedure would be quick and require just a few days of recovery.
“They told me I’d feel like a new woman. I feel like a bionic woman!” McArdle said in a 2016 promotional video shot shortly after the new valve was put in place.
Nearly three years later, she’s still feeling that good, she told the International Consortium of Investigative Journalists. “It was the most wonderful procedure. I didn’t have an ache in my body,” she said.
Aortic stenosis, a narrowed heart valve, is the third most common cardiovascular disease in the Western world. It often develops in old age, when open-surgery can be risky. TAVR has revolutionized treatment of aortic stenosis, extending the lives of hundreds of thousands of patients.
As its popularity has grown, doctors, with the strong encouragement of the manufacturers who make the valves, are using TAVR in younger and healthier patients. It’s common for medical devices to be used for different purposes or in different populations as the science advances, but for TAVR, a critical uncertainty remains: no one knows how long the valve will last.
The companies that make it, the researchers who study it and the doctors who spread its use around the world acknowledge that the TAVR valve’s durability is unknown. A consensus document written by four major heart societies in the U.S. has called for caution in treating patients who might outlive the device by decades.
We have no idea what the durability of those valves is, at all, period.
– Dr. Joseph Bavaria
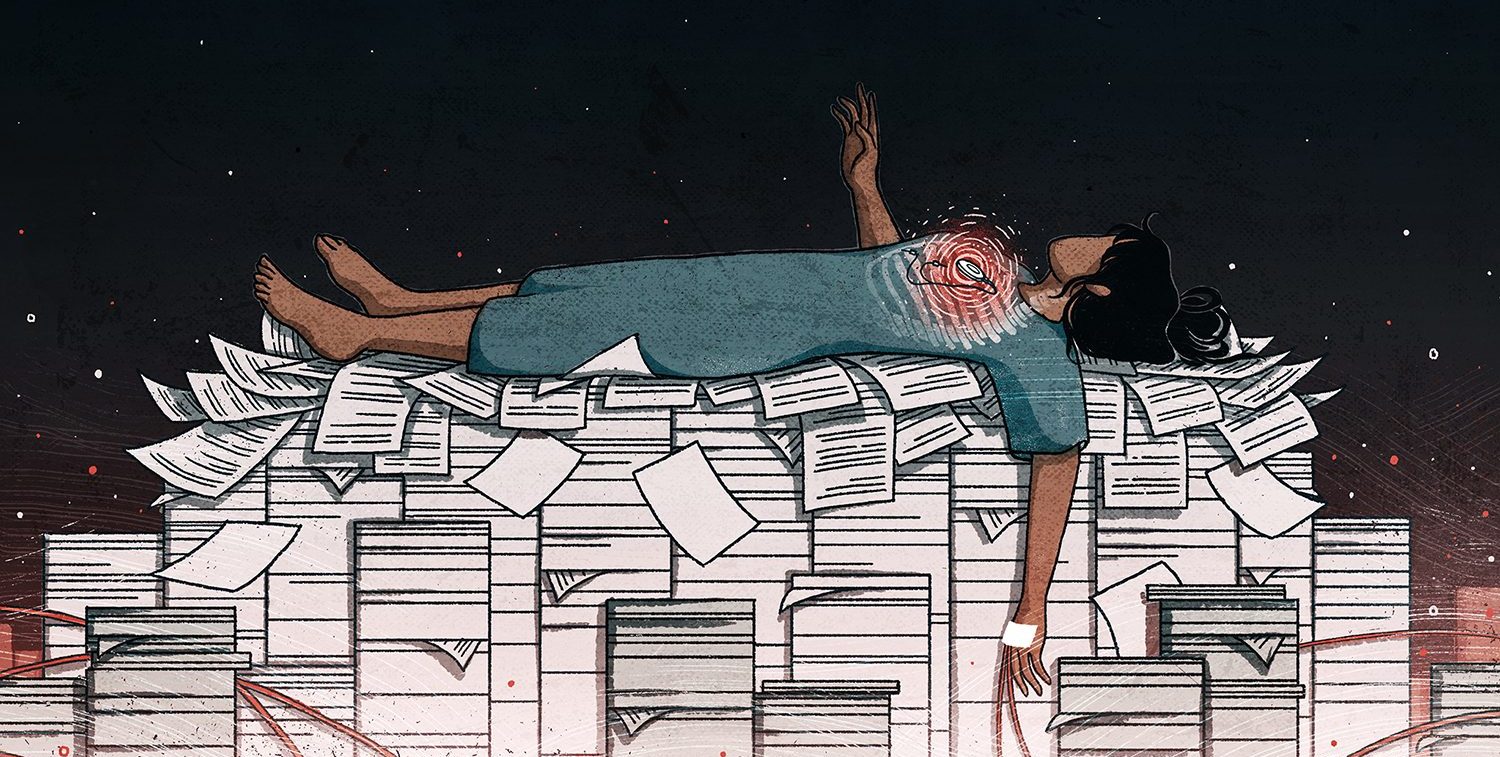
Doctors have told the International Consortium of Investigative Journalists that degradation of the TAVR valve may cause serious problems, including a need for open-heart surgery when patients are older, more frail and at greater risk of death or serious injury. Several studies have suggested that patients who are good candidates for surgical valve replacement have higher mortality rates if they receive a TAVR valve, instead.
At the same time, manufacturers have launched aggressive marketing campaigns targeting doctors, patients and advocacy groups. Both Edwards and Medtronic, the two manufacturers selling TAVR valves in the U.S., are bombarding cardiologists with ads touting their durability, even though there is no strong evidence that the valves last more than five years once implanted.
Learn more about the excellent durability of the SAPIEN 3 valve at booth 1915 at #TCT2018. pic.twitter.com/eJAFo6swRu
— Edwards Lifesciences (@EdwardsLifesci) 22 September 2018
Groups that claim to advocate for patients survive largely on industry money, and use human interest stories to sell TAVR to patients, politicians, and payers. Mended Hearts, a tax-exempt organization that provides support to hospitalized heart disease patients and their families through a visiting program and other peer-to-peer efforts, took more than a million dollars from pharmaceutical and device companies in 2016, including almost $300,000 from Edwards.
Patients are exposed to marketing campaigns targeting them everywhere, from their internet searches to their support groups, and doctors say patients often ask for or demand TAVR valves.
Edwards projects that the TAVR market will be $5 billion or more a year by 2021, driven by wider use, improved technology and increased “therapy awareness” – more patients asking their doctors about TAVR. Along with other manufacturers, Edwards sought to boost that awareness through patient groups, using them for direct-to-consumer marketing and as an effective tool for lobbying.
Mended Hearts, for instance, brings doctors and patients to explain the TAVR procedure at gatherings of heart disease sufferers, and their members appear in Edwards promotional videos. Mended Hearts members also speak to journalists and policymakers about the benefits of TAVR.
Just in the last few months, industry-backed lobbyists and patient groups have been pressing U.S. regulators to do away with limits on which hospitals can perform the TAVR procedure, and the government has separately agreed to pay for the procedure in a wider variety of patients.
“We have no idea what the durability of those valves is, at all, period,” said Joseph Bavaria, a doctor who co-directs the TAVR program at the University of Pennsylvania, where he is also a professor of surgery.
Bavaria is also chairman of the steering committee for the U.S. TAVR registry, a database of patient information and the outcomes of every TAVR procedure in the country. Many patients having TAVR are now from 65 to 75 years old, “and we don’t have a clue how these things work in those people.”
ICIJ spent the past year examining the medical device industry, its regulators, the doctors who use its products and the patients whose lives are changed — for better and worse — by medical technology. The investigation, known as the Implant Files, has uncovered many examples of devices approved with scant testing and devices allowed to remain on the market too long after their dangers have become clear.
TAVR is relatively early in its lifecycle. It has garnered widespread praise and enthusiasm, turning a previously dire diagnosis into a highly treatable condition. There is no question that it is helping people. Patients want it, and manufacturers want them to have it.
During McArdle’s surgical consultation, her doctors said she was in good shape and could have surgery, she recalled. But she insisted on TAVR. “I didn’t want surgery,” she told ICIJ. “I said, ‘If you have to cut me open, I won’t do it.’”
With such pressures, but without good data, clinicians have hard choices to make about the financial and medical risks and benefits for new kinds of patients. Those patients include younger ones who request or demand TAVR, with its relatively unknown risks, over open-heart surgery, with its obvious disadvantages.
As medical practice moves outside the patient populations for which there is data, clinicians and patients together must answer the fundamental question – who is TAVR for?
‘We can’t make 5 years go faster’
In the U.S., the Food & Drug Administration has approved TAVR for use in what it deems high- and medium-risk populations. This means, essentially, people at elevated risk of dying within 30 days of a surgical valve replacement.
Doctors in many countries are free to use devices, or drugs, for so-called off-label purposes, ones that regulators haven’t approved. Manufacturers, however, are forbidden to promote off-label uses, and governments and insurance companies often won’t pay for them.
In 2017, U.S. clinicians performed more than 900 TAVR procedures in low-risk patients in regular practice, not clinical trials. In 2015, the most recent year for which that data is available, 9 percent of German aortic valve replacement patients underwent TAVR because they asked for it, despite their probably not meeting approved criteria. Earlier this year, the U.S. government agreed to reimburse some TAVR centers for any low-risk patients that meet the criteria of ongoing clinical trials.

“We can’t make five years go faster,” said Vinod Thourani, chairman of the department of cardiac surgery at MedStar Heart & Vascular Institute and co-principal investigator of Edwards’ ongoing clinical trial of TAVR in good surgical candidates, commenting on whether it’s appropriate to use TAVR in patients who could theoretically outlive the new valve by decades.
“Whoever says we have the answer is wrong,” he told ICIJ.
In a statement to ICIJ, a spokesperson for Edwards wrote, “We have taken a disciplined approach to developing and introducing TAVR to patients in the U.S. and beyond, supporting it with evidence generated from a series of focused clinical trials. Our emphasis has been, and remains, on ensuring the best patient outcomes with this life‐saving therapy,” Edwards said in a statement to ICIJ. “Since CE Mark was first received in 2007, more than 350,000 patients have been successfully treated with [TAVR]. Data reports have supported the continued responsible introduction of TAVR, with an emphasis on high quality‐patient outcomes to guide the therapy development and expansion into new indications.”
Medtronic declined to answer specific questions from ICIJ. In a statement, the company said its TAVR system, called CoreValve, has been tested in “more than a dozen clinical trials,” which have confirmed the valve’s safety, efficacy and “durability out to at least five years.”
Medtronic published five-year data from its first big U.S. trial this year, which showed nearly identical mortality rates for surgical valve replacement and TAVR in patients who had at least a 15 percent risk of death during or shortly after surgery. The company recently published its first paper from an on-going trial comparing outcomes in lower-risk patients receiving either TAVR or surgery. It only included one year of follow-up data – the most they have so far.
Stent connection
One of the most interesting historical parallels to TAVR is the use of coronary stents, small mesh tubes that prop open clogged arteries. TAVR valves are made out of metal stents and animal tissue. Originally developed as a minimally invasive alternative to open-heart bypass surgery, stents quickly became a common treatment for stable patients with clogged arteries and, usually, chest pain during exertion.
Stent insertions cost insurers or uninsured patients around $25,000 in the U.S., although the bill can go as high as $70,000. One cardiologist, Samin Sharma of Mount Sinai Medical Center in New York, told ICIJ that he performs 1,600 procedures a year, including 1,200 stent insertions. His lucrative practice helped save the hospital when it was struggling in the mid-2000s, contributing about $180 million in revenue by 2006, according to Bloomberg Businessweek. Sharma has been well-rewarded for his efforts, reportedly making $4.8 million in 2012.
Startlingly, more than a decade of evidence shows that many stent recipients are unlikely to benefit more than similar patients treated with blood thinners or other drugs. And yet a million Americans receive coronary stent implants every year.
It’s not always a harmless intervention; stenting carries a small but significant risk of injury. About 2 percent of the 1 million U.S. patients a year who receive coronary stent implants will have serious complications such as bleeding. People with implanted stents are also at greater risk of serious complications in unrelated surgeries.
The first study challenging the perceived benefits of stents was published in 2007, leading to a drop-off in stent use. It also led to a year-long U.S. congressional investigation into the cozy relationships between manufacturers and doctors. A primary target of the investigation was the influential Cardiovascular Research Foundation, or CRF, which is led by doctors from Columbia University in New York, though it is not directly affiliated with the university.
In 2008, two senior U.S. senators, Herb Kohl, D-Wis., and Charles E. Grassley, R-Iowa, sent a letter to Columbia University. They asked for the financial disclosures of 20 doctors, including Martin Leon, co-founder of CRF and director of the Center for Interventional Vascular Therapy at Columbia, as part of a larger investigation into industry influence over coronary stent use and promotion.
A year later, the senators sent a letter saying that Leon’s disclosures failed to mention millions of dollars in payments and other income he received from medical device makers.

Leon still maintains close financial ties to industry. He has helped lead 50 clinical trials, according to the website for Triventures, a medical device venture capital firm he co-founded. Some of those trials have been for devices made by companies that Leon has equity in, including a heart stent made by Elixir Medical Corp, and Sentinel, a device used during TAVR procedures. The earliest reference ICIJ found to Leon’s equity in Elixir was in a presentation he gave a few months after the FDA approved the company’s stent for U.S. use.
It is unclear whether the unreported income mentioned in the senators’ letter included at least $6 million Leon reportedly received from Edwards Lifesciences when it bought a start-up he’d helped found, Percutaneous Valve Technologies. It was at PVT that Leon and his partners developed TAVR.
“The continued evolution of medical technology at Edwards remains dependent on these important relationships. In addition, physicians around the world rely on training and education sponsored by Edwards to help advance their understanding of the latest developments in medical techniques,” Edwards said in a statement to ICIJ. “The best trainers of physicians are usually other physicians, and Edwards is proud to provide funding to facilitate that.”
During the public debate about stents, Sharma’s stent insertions dropped from about 1,500 to 1,300 a year, Sharma told ICIJ, but his total number of transcatheter procedures is about the same now as it was in 2006. In 2010, he was one of three Mount Sinai cardiologists who together implanted the first Medtronic TAVR, CoreValve, in the U.S. He now performs about 150 TAVR procedures a year. His hospital has served as one of the primary sites for each of Medtronic’s TAVR clinical trials.
In an interview this year with ICIJ partners at EuroPCR, a medical conference in Paris, Leon defended doctor-manufacturer financial relationships, arguing that such partnerships spur innovation.
“I strongly believe that industry should be our partners,” he told reporters from Germany’s Norddeutscher Rundfunk and France’s Premieres Lignes. “They are the tool makers. We can advise them. We can help them conduct proper clinical trials. We can interpret the data in a very unbiased way, and we can develop the guidelines of how this new therapy shall be used.”
ICIJ sent Leon detailed questions about his financial relationships with Edwards and the device industry in general. In response, a Columbia spokesperson sent a statement outlining the history of TAVR in the U.S., including Leon’s role as one of the lead scientists on clinical trials that resulted in FDA approval of Edwards products. The manufacturer did not pay him for those leadership roles, according to the statement.
A treatment with less trauma
To understand the durability concerns, it helps to imagine a valve. In a healthy aortic valve, three thin tissue flaps called leaflets open and close with every heartbeat, starting and stopping the flow of blood into the aorta, which leads out to the rest of the body.
In the most common form of aortic stenosis, as patients get older the leaflets become encrusted with hard calcium deposits, which prevent them from opening fully. The narrower opening means the heart has to work harder to squeeze enough blood through to supply the body with oxygen. If the valve narrows enough, patients become oxygen-starved. Most cases are diagnosed because of shortness of breath, fatigue or chest pains.
Half of all patients with severe aortic stenosis will die in two or three years if they don’t get a valve replacement, though that calculation includes death from unrelated causes.
In surgical treatment, doctors crack open the ribcage, stop the heart briefly, cut out the natural valve and replace it with a prosthetic one. It’s clear why doctors went looking for a treatment without all that trauma and why patients are so eager to embrace it.
An artificial valve can either be made of animal tissue, known as a bioprosthesis, or materials like titanium and carbon, known as a mechanical valve. Bioprosthetics are less likely to cause blood clots, but patients’ immune systems, and the stress of beating 42 million times a year, inevitably break down those implants enough that they have to be replaced. About 20 percent of patients need a new bioprosthetic within 15 years. In general, the younger the patient, the faster the artificial valve’s function degenerates.
TAVR valves are metal stents lined with leaflets of pig or cow tissue. Depending on the type, cardiologists use a special press to squish the valve into a miniscule tube or “crimp” it around a tiny balloon. The whole package sits on the tip of a flexible catheter.
The doctor makes a small incision in either the chest or a leg artery and feeds the catheter straight into the heart, placing it inside the natural valve. She then blows up the balloon, forcing the valve open, or slides the tube off, letting it pop open. Unlike with surgery, the calcium-encrusted leaflets are never removed.
A TAVR valve could be less durable than a bioprosthetic surgical valve for a few reasons. TAVR leaflets are thinner than surgical valves and are subjected to serious mechanical stress. The pressing process can cause microscopic tears in the tissue, and being shoved through an artery is a hard journey. In computer simulations, TAVR longevity has come up short, compared with many surgical valves made with tissue.
Because aortic stenosis is often a disease of aging, many patients are too sick or old for surgery when they’re diagnosed. These patients were the original focus for Leon and his PVT co-founder, Alain Cribier, a cardiologist at Charles Nicolle Hospital of the University of Rouen, in France, when they began their company with two former Johnson & Johnson executives.
Cribier had been working on catheter-based valve procedures, and Leon had been heavily involved in stent research. Working together, they landed on the idea of placing leaflets in a metal stent and popping it open inside the patient’s diseased valve.
Cribier performed the first TAVR procedure in France in 2002. Two years later, Edwards Lifesciences bought the company for $125 million, including at least $6 million for Leon, according to Bloomberg Businessweek.
That first TAVR valve, which Edwards named the Sapien, went on to be approved in the U.S. based on clinical trials that Leon helped spearhead.
Seeking approval through Europe first
Edwards sought approval of TAVR first in the European Union, where even high-risk medical devices are approved by “notified bodies,” mostly private companies paid by the manufacturers. They decide whether to grant a “CE mark,” certification to enter the European market, to a broad range of manufactured products, including kitchen appliances, toys and medical devices.
The system has long drawn fire from critics, who argue that the process is too fast and too easy, with not enough safeguards. The CE mark doesn’t require clinical trials, where patients are assigned at random to the investigative treatment or the standard one, before devices are approved for sale and implanted in patients. (Though the U.S. system is frequently criticized for loopholes and lax enforcement, totally novel high-risk devices like TAVR are usually subjected to at least one “pivotal” trial before going on the market.)
As Edwards continued to develop the balloon-expanded TAVR conceived by Leon and his partners at PVT, Medtronic, the largest medical device company in the world, was in hot pursuit with a product that popped open itself. Both the Sapien and the Medtronic CoreValve received CE marks in 2007.
Many products, including TAVR valves, are sold first in Europe, and then brought to the U.S. once the kinks are worked out. Early TAVR patients had high mortality rates. Later streamlined, those bulky original valves were more likely to knock relatively large calcium pieces loose from native tissue, sending them into the bloodstream and potentially causing strokes. Between 2009 and 2010, when TAVR was still in its early stages in Germany, between 7.6 and 9.2 percent of all TAVR patients died during the hospital stay, a startling figure given that today’s mortality rates are around 2 percent in the U.S. and Germany.
“Although no single randomized controlled trial (RCT) was performed, [TAVR] was already applied in tens of thousands of patients,” Mattias Neyt of the Belgian Health Care Knowledge Center, told ICIJ. “Before high-risk medical devices [become] widespread, reliable evidence on their comparative safety and efficacy should be generated to establish the added value for patients.”
In an article published in 2013, Neyt and a co-author claimed that in the early stages of TAVR in Europe, arguments supporting expansion of the procedure did not stand up to scrutiny.
In the U.S., the FDA did require TAVR to undergo clinical trials, which Leon helped run. He was also a key figure in each of Edwards’ subsequent TAVR trials.
In that first U.S. trial, the TAVR recipients had an 11.2 percent stroke rate in the first year, compared with a 4.5 percent rate in the surgical valve group. Patients receiving the transcatheter valve were also more likely to have significant bleeding.
At the 2011 FDA panel discussion about approving the device, one speaker, Steven Greer, a health-care analyst who trained as a surgeon, compared TAVR to another product approved based on clinical trials run by Leon. It was a drug-coated stent that released medication after insertion in an effort to prevent one of the most common complications. Millions of patients received drug-coated stents, and then complications arose that could lead to death or injury years after the procedure.
“A perfect storm is brewing, creating a major public hazard,” Greer told the FDA panel, speaking of TAVR.
“The evaluation and introduction of the transcatheter heart valve therapy was painstaking, with rigorous, objective criteria prespecified in [U.S.] studies, a complex and thorough regulatory pathway and a focus on high quality patient outcomes,” Edwards said in its statement to ICIJ.
The FDA approved the Sapien in 2011, and Medtronic’s TAVR device, CoreValve, nearly three years later. Both approvals were only for high-risk patients.
Widening use of the devices
Though in the U.S., manufacturers aren’t allowed to advertise their products outside the bounds set by federal regulators, doctors in the U.S. and in many other countries, can use devices in whatever ways they believe to be medically necessary. This is called off-label use.

Doctors have used TAVR off-label since the early days. In one study, independent cardiologists looked at medical records from a German municipal hospital between 2009 and 2012, when TAVR was approved only for patients at high risk of dying during or shortly after surgery. Of 185 patients implanted with TAVR valves, only a third were high-risk. The other two-thirds were split evenly between low- and medium-risk.
In the interview with ICIJ’s partners Norddeutscher Rundfunk and Premieres Lignes, Leon said TAVR devices have improved dramatically over time. The TAVR device “has gotten smaller, much more predictable. Many of the inconsistencies are gone,” he said. “The complication rates have gone down.”
In 2015, Leon was a step ahead of the FDA, arguing that doctors should already be considering TAVR first for so-called intermediate-risk patients, who have a predicted 4 percent to 8 percent risk of dying during or soon after surgery.
“The conversation needs to change. We have checked the boxes for low-risk patients,” Leon told that year’s annual European Society of Cardiology meeting, according to the Medscape website. “We used to ask: who does poorly with [open-heart surgery]? That question should change to: who does well with TAVI?” TAVR is also known as “transcatheter aortic valve implantation,” or TAVI.
One of Leon’s primary arguments, according to his presentation slides: Doctors were already using TAVR regularly in those lower-risk patients, both in the U.S. and in Europe.
In response to questions about the presentation, a spokesperson for Columbia said Leon’s argument was borne out by later evidence. And, indeed, the FDA approved the indication a year later in 2016, based on trials Leon helped design and run.
According to the written statement Columbia University provided to ICIJ, “Dr. Leon and most other leaders in the TAVR field have strongly advocated not treating low-risk patients with TAVR, other than in the context of an FDA-monitored clinical trial.” Neither Leon nor the spokesperson responded to specific questions about the 2015 presentation.
Both Edwards and Medtronic are hoping to present one-year data from their ongoing clinical trials in low-risk patients next year. Edwards has been telling investors to expect FDA approval late next year.
The FDA, meanwhile, has recently approved so-called “continued access” trials for the Sapien 3 and the Evolut R, the most recent Edwards and Medtronic TAVR valves, based on a review of early data from ongoing trials. That means some institutions will be able to use TAVR in any low-risk patients they deem appropriate.
Sharma, at Mount Sinai, is one of the clinicians granted that discretion. He acknowledged to ICIJ that there are reasons to be cautious, including several studies suggesting low-risk patients might have higher long-term mortality if they have TAVR instead of surgery.
But, he argued, if there had been a mortality difference in the early results, the FDA wouldn’t have allowed the continued access trial.
Next year, the FDA will make its decision about approving TAVR in low-risk patients based on only one year of data. The trial participants will be tracked for 10 years, but if the procedure is approved, the national registry will track regular recipients for only one year. Eventually, researchers hope to connect the registry with other databases, including Medicare and the national death database, to find out what’s happening with these patients over time.
Bavaria, chairman of the steering committee for the U.S. TAVR registry, said caution has prevailed – at least in the U.S. “This is one of the few things we’ve actually done rationally. We did good here,” he told ICIJ. “We’re providing access, but not at the expense of quality.”
TAVR is not very profitable in the U.S. right now. But in Germany, according to both clinical and policy experts, hospitals make more money on TAVR than surgery. And German patients receive far more TAVR valves, proportionally, than American patients do.
In the U.S., the number of TAVR procedures jumped from 4,600 in 2012, the first full year after FDA approval, to nearly 35,000 in 2016. In Germany, which has a fourth as many people as the U.S., the number of TAVR procedures exceeded 17,000 in 2016.
“We have a supply-driven expansion of TAVI in Germany right now, which cannot solely be explained by medical reasons, but clearly has monetary reasons, too,” said Josef Hecken, chairman of the Federal Joint Committee (Gemeinsamer Bundesausschuss), a body that decides which services are covered by German health insurance, among other things. “In my opinion, except for inoperable or high-risk patients, TAVR has not yet proven superiority to the surgical valve replacement.”
Debate: What does the data support?
Durability is not a new conversation for interventional cardiology.
In May 2016, Canadian cardiologist Danny Dvir, of St. Paul’s Hospital in Vancouver, British Columbia, shook up the cardiology community at a European conference. He presented data showing that within eight years, 50 percent of early TAVR valve recipients had valve deterioration that either re-created aortic stenosis or leaked blood backward, which can result in significant stress on the heart.
The study had a number of limits, including that only a few early patients were still alive after eight years. Some cardiologists also questioned whether the data was applicable to newer valve models, such as the Sapien XT, which was approved in 2014.
Regardless, the presentation sparked debate about TAVR expansion and the lack of durability data. That July, TCTMD, a newsletter of the Cardiovascular Research Foundation, published a conversation involving 16 prominent TAVR doctors about what to do when low-risk patients insisted on having TAVR instead of open-heart surgery.
There are enough uncertainties about durability that it won’t be ethical to use it in low-risk patients until careful long-term data is available.
– Dr. Gregg Stone
Dr. Gregg Stone, then CRF’s director of medical research and now its president, said it would be unethical to provide TAVR as an option for low-risk patients, even those well-informed of the risks, given the lack of data.
“I don’t believe we can ethically justify implanting a device in such a scenario not yet supported by evidence-based medicine just because funding is available,” he wrote. “There are enough uncertainties about durability that it won’t be ethical to use it in low-risk patients until careful long-term data is available from randomized trials, including in studies comparing surgical valves to TAVR in younger patients.”
At the same conference where Dvir presented his data, at least one doctor said his institution was regularly using the device in low-risk patients. Andreas Baumbach, a cardiologist at the Bristol Heart Institute in the U.K., complained that, in medicine, often “the discussions and guidelines and evidence [come] way behind the clinical practice. We’ve been doing lower-risk patients for so long, and, in everyday practice, it’s become the norm. Here we are still discussing it.”
Research since then has been conflicted, and a recent paper, following older recipients for eight years, found much lower rates of deterioration. But the real question, according to experts, is how the valve fares in younger and healthier patients and what that means for their health long-term.
One study, earlier this year, analyzed data from almost 3,500 low-risk patients in the U.S. and found higher rates of mortality at two years for good surgical replacement candidates who got TAVR instead. An Italian study of low- and intermediate-risk patients also found lower survival rates in those who received TAVR, beginning at two years. The mortality gap has continued to increase through five years, the last year for which data is available.
There are limits to these studies, especially because they involve older generations of TAVR. But experts who reviewed data for ICIJ expressed concern that the FDA will decide whether to approve TAVR for low-risk surgical candidates based on just one year of follow-up data.
Sharma, one of the investigators in Medtronic’s ongoing trial of TAVR for good surgical candidates, and Thourani, the co-principal investigator of Edwards’ ongoing low-risk trial, both told ICIJ that it will be years before they can conclusively say TAVR is durable enough for use in younger, low-risk patients. Both now use it in low-risk patients they believe are good candidates, as part of the continued access trials.
Meanwhile, in September, at the Cardiovascular Research Foundation’s biggest conference, Transcatheter Therapeutics, or TCT, device makers were openly proclaiming TAVR’s durability. TV screens played looped Edwards ads boasting of its latest TAVR valve’s “excellent durability” – based on “20 years of simulated wear” in company laboratory tests. Conference workers handed out the day’s agenda with an ad for Medtronic’s newest TAVR valve printed on the front and back. The campaign’s slogan, “meaningful means a valve designed for durability,” appeared over a photo of an older couple dancing on a beach.
ICIJ asked Thourani about another Edwards ad, which used his one-year data to market TAVR valves’ durability to cardiologists, including those who don’t have his insider knowledge and context. Thourani said he was pleased to see that the fine print clarified how short the follow-up was.
“You and I aren’t going to change capitalism,” he said. “We should concentrate on peer-reviewed data.”
The direct approach
Doctors aren’t the only marketing targets for Edwards and other manufacturers. Many Edwards-funded educational resources remind patients that they have the right to a second opinion about the best medical option and offer a toll-free hotline to help patients find a TAVR doctor. They are widely disseminated to patients through Google ad campaigns and organizations like Mended Hearts, the group that takes hundreds of thousands of dollars a year from Edwards.
Several clinicians told ICIJ that patients routinely expect to receive a TAVR valve, whether or not it’s appropriate.

A small incision is, of course, an easy thing to sell to patients when the alternative is having their chests cracked open. “Patients, of course, they Google, they’re informed, and they ask for advice. Clearly this direct-to-consumer advertising makes a difference,” said Dr. Art Sedrakyan, the director of the Coordinating and Science Infrastructure Center at the Medical Device Epidemiology Network, a public-private initiative of the FDA. He is also a professor of health-care policy and research at Weill Cornell Medical College in New York.
“Clearly industry wants to sell their products,” Sedrakyan told ICIJ. “It’s our role in academia to raise this flag and highlight the uncertainties and lack of evidence.” And in the meantime, he said, clinicians have to be honest with patients about the risks.
Patients have served as powerful allies in device makers’ campaigns to expand approved uses and reimbursement for TAVR. Groups like Mended Hearts often serve as the conduit for that energy.
In response to detailed questions from ICIJ about the group’s entanglement with Edwards and other manufacturers, Mended Hearts sent a short statement.
“We consistently encourage patients to make medical decisions based on their individual needs and discussions with their doctor,” a spokesperson wrote. “Mended Hearts is proud of the relationships we have built with medical providers and professionals, hospital systems and industry partners. While these partnerships allow us to provide patients with the most current and relevant information available, Mended Hearts has always remained independent of all industry influence and is transparent about our partnerships and programs.”
Mended Hearts is part of the Heart Valve Disease Policy Task Force, an Edwards-funded umbrella group of organizations that also receive funding from other TAVR manufacturers for some campaigns. The group says its goal is to “improve access, research and awareness on heart valve disease detection and treatment,” but a primary focus is expanding the use of TAVR.
The campaigns, which often stress the common-sense desire to avoid open-heart surgery, include a form letter patients have been encouraged to send to a Canadian health minister in an effort to increase government spending on TAVR.
“If you were faced with the choice of having your chest broken open to repair your heart, undergoing surgery under general anesthesia, followed by a lengthy hospital stay and up to several months recovering at home, or a less invasive procedure using local anesthetic that can see you walking within hours, home within a few days and feeling better than you did before within weeks, which would you choose?” the form letter asks.
According to the campaign, thousands of letters have been sent so far.
The task force is headed by a group called the Alliance for Aging Research, whose board members are almost entirely drug and device industry leaders and lobbyists. Seven board members are current or former industry executives, including Barry Liden, vice president of patient engagement at Edwards, and Bruce Garren, Edwards’ former vice president of public affairs.
Two board members specialize in marketing drugs and devices to patients through advocacy groups, and two others are former U.S. Congress members who now lobby for the medical industry. One of them, former Rep. Billy Tauzin, resigned from Congress and immediately took over as CEO and top lobbyist of the main pharmaceutical lobbying group, PhRMA. He is now an independent health-care lobbyist.
A spokesperson for the Alliance for Aging Research declined to answer detailed questions from ICIJ.
“Patients continue to struggle to get access to information about their options or medical treatment,” Edwards said in a statement. “That is why we publicly support patient groups like Mended Hearts, the Heart Valve Disease Policy Task Force and others, who work with patients to educate patients about the disease and ALL of their therapy options, and the risks and benefits of each. Our support of patient groups is not contingent on or connected to any specific product or brand, or any specific public policies,” Edwards said. “Our support is intended to empower patients to use their experience to help themselves, encourage patients to talk to their doctors and to build a community of patients who care about making a difference.”
According to a document Mended Hearts distributed to volunteers this year, Edwards gave the organization a grant to support visiting TAVR patients in the hospital and “raise awareness of this innovative valve therapy during regional and national educational programs.”
The volume question
The debate over TAVR valve durability is not the only one in which industry influence appears to complicate the discussion of patient safety.
When the agency that administers Medicare, the U.S. government insurance for older patients, agreed to pay for transcatheter valve replacements, only hospitals that performed 20 TAVR procedures a year could bill the government for it. That’s because hospitals – and doctors – with less experience in TAVR and similar procedures generally have much worse outcomes.
German regulators are considering volume requirements in response to research showing higher mortality rates at centers with fewer patients.
In June this year, U.S. regulators put out a call for public comment about the coverage rules. At least seven of the 95 comments came from Mended Hearts members, some of whom used language drawn from a Heart Valve Disease Policy Task Force campaign, which demands “access to ALL appropriate treatments for ALL heart valve disease patients.”
The task force brought patients to Washington to meet with lawmakers and ask them to support coverage of the procedures at more hospitals. It also hosted a briefing on Capitol Hill to make the case that rural patients are unfairly harmed by lack of access to TAVR.
“Volume is no longer a necessary surrogate for health outcomes in hospitals that offer TAVR,” wrote Sue Peschin, CEO of the Alliance for Aging Research, in an opinion piece for The Hill, a newspaper that focuses on Congress and U.S. politics. “[Medicare] should work with independent partners on survey research to better understand what patients, not just doctors, prefer.”
At a public hearing in July, several advocacy group members spoke in favor of easing TAVR volume requirements. Mended Hearts’ president, Donnette Smith, disclosed receiving payment as a “consultant to Edwards Lifesciences” on TAVR and surgical valve replacement. She gave a joint presentation with the head of another task force member group, Heart Valve Voice, who disclosed receiving funding from Edwards and Medtronic, as well as Abbott, which has a TAVR valve in clinical trials.
They argued the same thing Edwards’ presenter did: that volume is a bad surrogate for quality, and better ways to judge a center’s outcomes are urgently needed.
In stark contrast to those presentations, four major U.S. heart societies published joint guidelines earlier this year, which Bavaria co-wrote. The guidelines call on Medicare to raise the cut-off from 20 to 50 TAVR procedures a year, as a way to help keep patients safe while researchers develop better ways to measure quality.
At this year’s TCT in September, Bavaria and CRF founder Leon both took part in a panel debate on hospital volume.
Bavaria pulled no punches in his presentation.
“This is the most recent, comprehensive data set on the globe today,” he said, flipping through slides with patient outcomes data from the U.S. and international TAVR registries. Together, they led to an inescapable conclusion: centers performing fewer than 50 TAVR procedures a year are likely to have significantly higher mortality rates and serious complications than centers with greater volume.
“It doesn’t take a rocket scientist to figure out that we have a volume-outcome relationship here. It’s like denying the Holocaust,” Bavaria said.
Then Leon offered the counterpoint. “I hope at the end of this I’ll be a Holocaust survivor,” he joked.
“We all want optimal clinical outcomes for our patients, that’s obvious,” Leon told the audience. “We recognize that to achieve optimal access, which means everyone – that may be unrealistic.. There may be a need to balance which sacrifices the highest quality under certain circumstances.”
He pointed out that raising the cutoff to 50 would threaten to exclude current TAVR sites. Those hospitals, he said, would end up doing however many procedures they needed to meet the threshold.
“I know how sites behave. I know how our health system works. If you cannot fulfill the [Medicare] requirements,” Leon said, “then you start making arbitrary decisions on how you take care of patients to achieve that level. And that’s not the way we should behave.”
ICIJ spoke with Bavaria after the panel. He clarified that he likes TAVR and performs it himself on patients he thinks it’s appropriate for. But he said he approaches this new technology, like any new technology, with caution.
“It’s a little strange to be advocating for low-volume centers when none of the people in that room would ever go to a low-volume center,” Bavaria told ICIJ. “To us, individual quality trumps access.”
Ultimately, the story of TAVR comes down to a question of risk tolerance. Is access more important than having the best outcomes at each center? If a patient wants to leave the hospital “with a Band-Aid,” as Jeanne McArdle, the overjoyed TAVR recipient, told the world she had in her TAVR promotional video, does it outweigh a clinician’s concerns about what will happen a decade down the line?
Many experts have their own answers.
“I, personally, wouldn’t want a TAVR if I were low-risk right now,” Bavaria told ICIJ. “We’ll find out, won’t we?”
Contributors: Elena Kuch and Edouard Perrin